If you have seen my recent posts on LinkedIn you probably know that I am looking to interact with healthcare professionals to brainstorm ideas on how Triage can be improved. In this post I will cover what Triage is and some common issues identified with the process and my attempt at a solution. I am hoping this post will help get the ball rolling and get others to help come up with innovative solutions.
What is Triage?
Put simply Triage is a process used to identify and prioritize Patients in need of care. This is important since every year there are 100’s of events where people get injured or an epidemic spreads that require hospital staff to respond. Often Paramedics and Doctors are expected to provide care for hundreds of victims but provided with few available resources like hospital beds and ambulances etc. Triage is not a new concept and seems to have origins in the Napoleonic wars. In fact even today Triage is most commonly practiced on the battlefield.
Triage has a number of different processes that are followed by different countries however there are a few common elements. Typically a patient is categorized based on the criticality of the injury into 1 of 5 groups. They are defined loosely below
- Expectant – People who will die regardless of what treatment they receive.
- Immediate or Emergency – people who will die if not treated within 60 minutes
- Urgent – People whose injuries are severe but not life threating in the short term
- Semi Urgent or Delayed – People whose injuries are not severe but are in need or medical care.
- Non Urgent – People who are not in need of medical care that requires a visit to hospital.
What’s wrong with the current system?
Here is a small list compiled to name a few common problems identified with systems that are in place now
- Under Triage: – Miscategorizing people in need of say urgent care as Semi Urgent, this denies a patient the proper care based on their condition.
- Over Triage :- Miscategorizing people in need of Semi Urgent care as Urgent, resulting in shortage of critical care facilities to people who are in immediate need of it , such as hospital beds , blood , OT rooms etc.
- No Patient specific details: – A young person is more likely to survive burns compared to an older person but this is not a factor for categorizing the patient.
- No Hospital capabilities: – Patients are sent to hospitals that may or may not have the required facilities.
- Geographic distribution: – Not factoring in the number of other hospitals available within a reasonable geographic distance.
- Walking Wounded:- During Mass attacks a significant number of walking wounded find their way to nearby ERs overwhelming them while they are expecting more critically injured.
What is being proposed?
In order to arrive at this solution, I basically went with the below goals that the Triage methodology should be able to meet
- Get healthcare to as many people as possible.
- Get healthcare faster to those who need it most.
- Identify and streamline patient and deceased information and track progress through the system
- Be simple enough to be implemented with minimal training
- Be flexible to handle 10s to 1000s of patients by illness.
- Be Global
So here is the solutions I came up with graphically
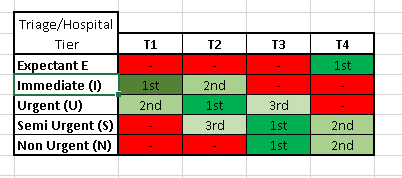
You will notice that it’s a matrix where the y axis has the standard criteria for judging the criticality of the injury but on the x axis we have hospitals that are tiered based on facilities.
While I am not an expert here is how I see the hospitals being tiered.
T4– Basic clinics or hospitals that are typically 8-10 km away from the site and provide basic treatment like IV, morphine, and can at most take X-Rays.
T3– Hospitals within 8 kms that can provide T4 and has at least 10 beds + basic lab facilities to further help diagnosis and provide minor care. T3 hospitals might have a minor OT for treating minor burn, fractures, amputations etc.
T2– Hospitals that are typically less than 5 km away and can provide complete care including minor and major surgery but probably are not staffed as well as T1 or have limited number of specialized departments.
T1– Hospitals that can provide the entire set of care need for any possible emergency, usually these hospitals get grants from Govt. for elevated level of preparedness.
Within the cells you will see that every combination of Hospital Tier and Severity has a preference associated with it which is determined by the paramedic or Doctor. Say for example in the event of earthquake first responders arrive at the site and are faced with hundreds of people under collapsed buildings
A person with gash on the head and bleeding profusely but able to walk might be N3 and unable to walk might be S3
A person with who is unconscious but not showing signs of physical trauma might be S3 but with physical Trauma might be S2 or if the patient is an infant or elderly person then U3
This way, when there is ambiguity there is a default preference for each combination of the tier while still allowing room within the process to bump up or down the patient based on survivability.
Sections marked in RED are cases that are not allowed e.g. Expectant patients are never taken to T1 hospitals.
While above system is the methodology there are a few additional assumptions that need to be made. These are as follows:-
- All hospitals need to be part of the network and should be categorized
- A T1 hospital should be made available within 5 km or 10 minutes anywhere in the city that average over 20,000 people a day, e.g. Airports, Shopping districts, Stadiums etc.
- Patient identification and admission should be performed “on site” and not at the hospital, smart card system identifying patient, nature of illness, photo is possible as well as assigned hospital, collect as much patient info at source to aid identification later on.
- National register showing capacity and capability for each hospital
- First aid to be taught mandatorily at school level, additional merit and recognition for those who know it in job interviews, Govt. service recruitments etc.
Advantages
T1 Hospitals are not flooded with patients just because they have capacity. We allow some room in case of subsequent events like aftershocks, Tsunamis, a second bomb etc.
Based on typical distribution patterns a city is most likely to have more t2 and T3 hospitals and the Triage process takes advantage of it by redirecting more patients there.
Accommodates Patient level, Hospital level and Criticality level information to a lot care.
First Responder has only 10 possible combinations to use. Which should become second nature with practice.
Brings into scope much more hospitals thereby increasing likely hood that everybody gets the care they actually need
Disadvantages
Might be more complicated than some systems already in place (but it might more effective).
Driven by external factors like Govt Involvement.
Strongly relies on capability of first responder to Triage properly.
Naturally I would love to hear any other advantage / disadvantages that I haven’t thought of. Please note I am not pretending to be an expert or saying I have a solution I am just thinking differently and would like to know if the idea has any merit and could one day maybe save my own life.
Please Consider Subscribing